Same Day Online ADHD Diagnosis
ADHD assessment?
Women with ADHD face unique challenges when it comes to stress management. Fluctuating hormone levels, executive dysfunction, and disrupted eating patterns can all contribute to elevated cortisol—a stress hormone linked to fatigue, anxiety, and long-term health complications. The good news? There are natural, sustainable ways to manage stress and regulate cortisol levels—starting with nutrition, routine, and self-awareness.
We spoke with a variety of registered dietitians, nutritionists, and health experts to uncover evidence-based, practical strategies specifically tailored for women navigating ADHD.
1. Fuel Your Brain with Steady, Nutrient-Dense Meals
One of the most consistent pieces of advice from experts is simple: don't skip meals.
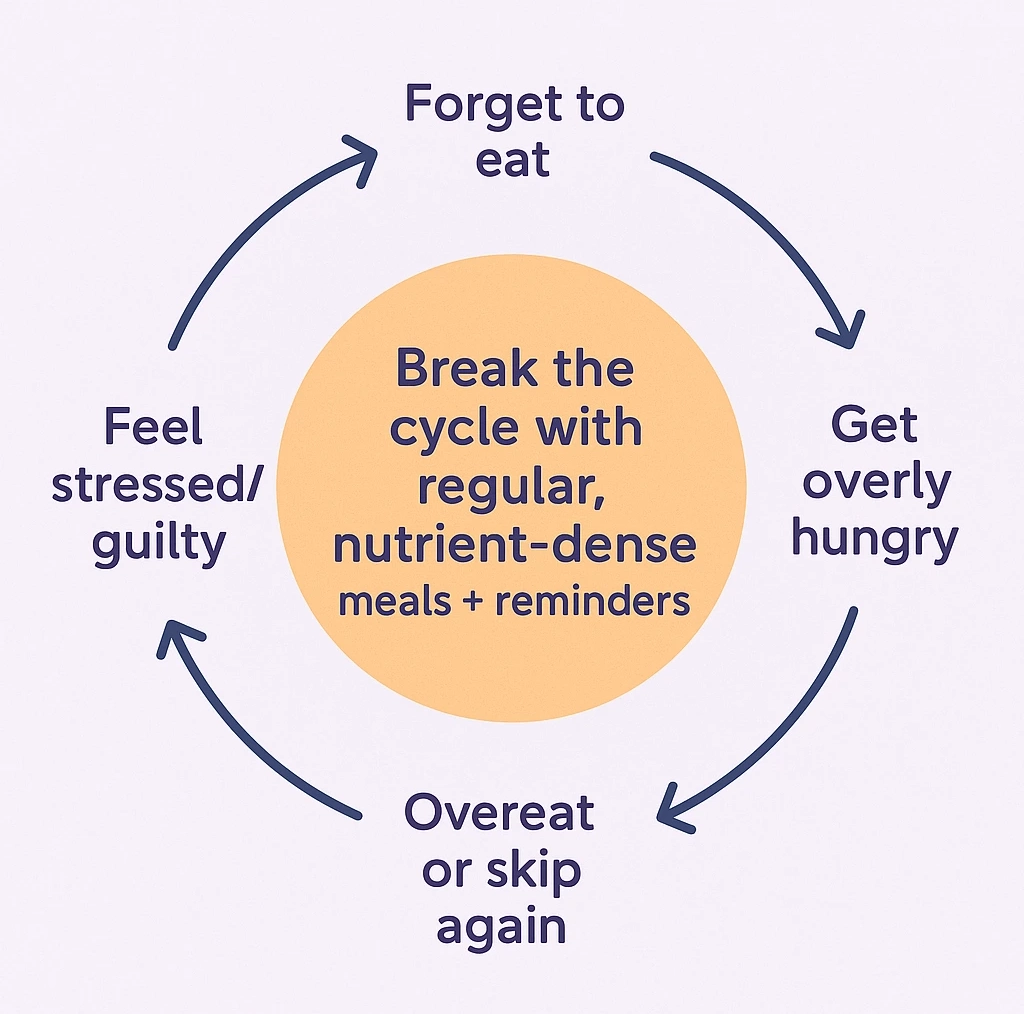
According to Heather Fiore, MS Ed, RD, LD, CDCES, a weight-inclusive, HAES-informed anti-diet dietitian at Free State Nutrition, one of the most common pitfalls for women with ADHD is “forgetting to eat until they are absolutely starving.” Fiore explains that ADHD can interfere with recognizing hunger cues, and when paired with executive dysfunction, making food choices becomes overwhelming. “Stress levels are generally improved with adequate nutrition,” she notes.
To avoid this pattern, Fiore recommends setting reminders for meals and snacks. “The foods themselves are not nearly as important as the adequacy,” she says. Start with quick, easy meals and supplement with grab-and-go snacks to build consistency and reduce stress.
2. Choose Foods That Calm, Not Trigger
Valerie Goldstein, MS, RD, CDCES of Thrivelab, emphasizes that cortisol regulation can be significantly improved through diet. She recommends dividing your daily intake into six small meals, each containing protein, plant-based carbohydrates (like fruit or legumes), and healthy fats. “Eat foods that do not antagonize cortisol release,” she advises.
Goldstein suggests including foods such as:
- Fatty fish like salmon
- Leafy greens
- Berries
- Fermented foods (kimchi, sauerkraut, apple cider vinegar)
- Dark chocolate (90–100% cocoa with <10g sugar)
- Sweet potatoes, lentils, beans, and nuts
To support hydration and mineral balance, she also recommends adding a teaspoon of Celtic sea salt to meals and eating every few hours to stabilize blood sugar and energy.

3. Reduce Inflammatory Foods
Many experts agree that what you avoid is just as important as what you eat.
Shelley Balls, MDA, RDN, LDN, a registered dietitian with Flawless Bloom, warns against excessive consumption of ultra-processed foods. “They’re high in sodium, simple carbohydrates, and solid fats—all of which negatively impact mental well-being,” she says. Balls adds that excess sodium can increase anxiety, and processed sugars spike blood glucose levels, triggering stress and inflammation.
According to Balls, foods to limit include:
- Pastries, sweets, and sweetened drinks
- Fried foods and processed snacks
- High-mercury seafood
- Red meat, butter, and excessive cheese
These foods can disrupt gut health and worsen mood swings, making ADHD symptoms more intense.

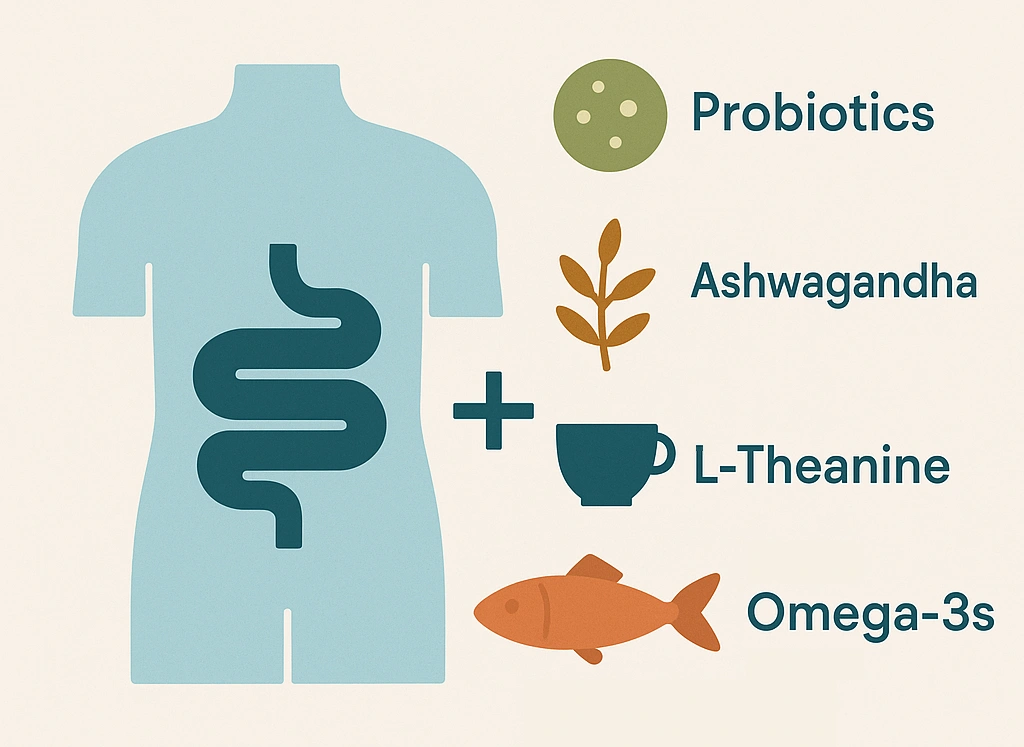
4. Focus on Gut Health & Key Nutrients
Your gut and brain are intimately connected, and nurturing gut health can be a powerful way to reduce stress and cortisol.
Goldstein highlights the value of probiotics like Bifidobacterium longum 1714, Lactobacillus acidophilus Rosell-52, Lactobacillus plantarum 299v, and Lactobacillus casei Shirota, which may positively influence the nervous system. She also recommends ashwagandha, a natural adaptogen shown to reduce cortisol levels, and L-Theanine, found in green tea or herbal blends like Whispering Wildflowers™.
Balls concurs, noting that probiotic-rich foods such as kefir, yogurt, and tempeh help support a healthier stress response and cognitive function. Other standout nutrients she recommends include:
- Omega-3s (salmon, mackerel)
- Magnesium (pumpkin seeds, leafy greens)
- Vitamin D, zinc, and antioxidants
5. Create Routines and Pair Nutrition with Lifestyle Tools
A structured routine complements dietary changes. Larry Johnson, a health and wellness writer with Dune Medical Devices Inc., emphasizes that pairing dietary shifts with daily structure amplifies their effects. “Structured routines—a principle emphasized by Dune’s patient-centered approach—can bridge nutrition and mental health.”
Johnson also notes that omega-3s from fish can reduce cortisol and inflammation while improving focus, and magnesium-rich foods like pumpkin seeds can promote relaxation.
Goldstein underscores the value of pairing gentle movement with mindfulness practices. “Move your body, relax your mind,” she says, recommending meditative tools like Sarah Raymond’s Mindful Movement to activate the vagus nerve and regulate the nervous system.

ADHD, Cortisol, and the Female Brain: Why It’s Different
While everyone experiences stress, women with ADHD often face a double burden due to the intersection of neurological and hormonal dynamics.
Research shows that estrogen and progesterone directly influence dopamine regulation, which is already dysregulated in ADHD. This hormonal fluctuation—especially around menstruation, perimenopause, and menopause can exacerbate both ADHD symptoms and stress sensitivity. Simultaneously, cortisol, the primary stress hormone, becomes more reactive under chronic stress and fluctuating blood sugar—two common challenges for women with ADHD.
For women with ADHD, managing cortisol isn't just about stress, it's about stabilizing an already sensitive internal environment. That’s why supporting the nervous system nutritionally and behaviorally is essential.
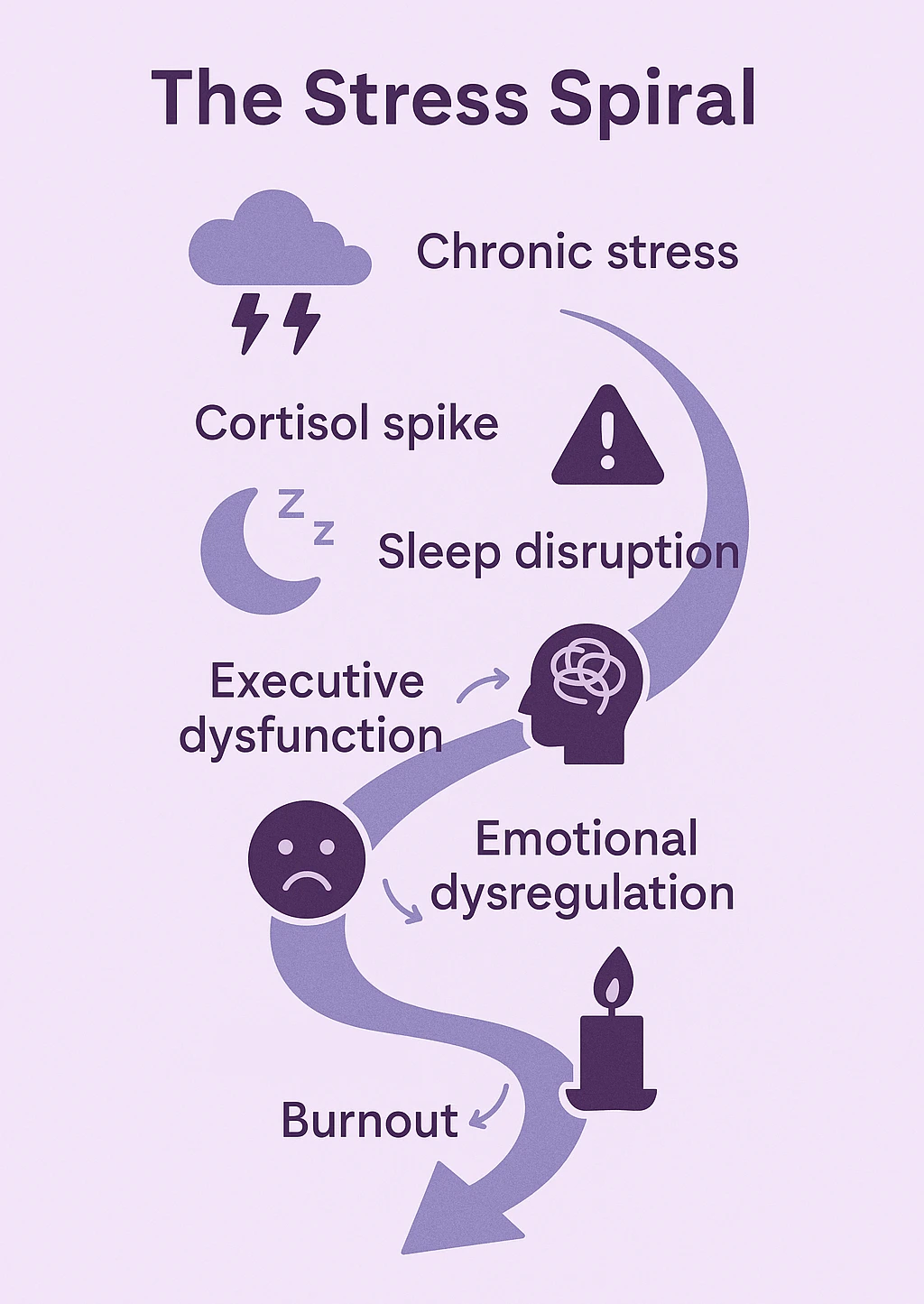
How Chronic Stress Impacts ADHD Symptoms
Chronic stress, and the cortisol overload that comes with it, can make ADHD symptoms worse. Elevated cortisol has been associated with:
- Reduced working memory and slower processing speed
- Sleep disruption, which further worsens focus and mood
- Impaired decision-making and executive functioning
In people with ADHD, the prefrontal cortex is already under strain. Add elevated cortisol, and it can feel like the brain is constantly in “fight or flight” mode, making emotional regulation, organization, and attention even more difficult.
The good news? Targeted lifestyle strategies (like those shared by our experts) can help reduce this load and restore cognitive flexibility over time.
How Long Does It Take to See Results?
One of the most common questions is “How fast will I feel better?” While individual results vary, here's a general timeline based on clinical nutrition literature and behavioral studies:
- Within a week: Blood sugar stabilization can reduce mood swings and brain fog.
- 2–4 weeks: Gut health improvements (especially with probiotics and fiber) begin to modulate stress response.
- 4–8 weeks: Omega-3s and adaptogens like ashwagandha may begin to noticeably reduce cortisol and improve focus.
- Ongoing: Consistent structure, mindful eating, and routine movement help reinforce the brain-body connection and create long-term stress resilience.
Setting realistic expectations is key. These strategies aren't quick fixes, but when practiced consistently, they lead to sustainable improvements in both stress levels and ADHD management.
Understanding ADHD in Women
ADHD in women is often underdiagnosed or misdiagnosed, largely because symptoms tend to manifest differently than they do in men and boys. While hyperactivity is commonly recognized in childhood ADHD—especially among males—women are more likely to present with inattentive symptoms such as disorganization, mental fatigue, forgetfulness, emotional sensitivity, and chronic overwhelm. These subtle signs are frequently misunderstood as character flaws or anxiety rather than a neurodevelopmental condition, leading many women to go undiagnosed until adulthood. Hormonal fluctuations across the menstrual cycle, pregnancy, and menopause can further intensify symptoms, making stress regulation and emotional resilience even more challenging.
In adulthood, the toll of untreated or poorly managed ADHD can be significant. Women with ADHD are more likely to experience co-occurring mental health conditions, including anxiety, depression, and low self-esteem. The constant mental juggling act—combined with societal expectations around productivity, caregiving, and emotional regulation—can lead to burnout. Fortunately, greater awareness and access to targeted support, including lifestyle interventions, therapy, and telehealth evaluations, are helping more women recognize their symptoms and find effective strategies to thrive.
How to Get ADHD Support and Diagnosis Through ADHDAdvisor.org
ADHDAdvisor.org provides a streamlined process to help individuals seek ADHD evaluation and ongoing support from the comfort of their homes. Here's how you can get started:
1. Initial Symptom Screening
Begin by completing a free online assessment that screens for ADHD, anxiety, and depression. This helps determine if a clinical evaluation is recommended.
2. Connect with a Licensed Provider
If the screening suggests further evaluation, you'll be matched with a licensed mental health professional in your state. Appointments are available seven days a week, including evenings, with same-day options in many cases.
3. Clinical Evaluation
During a secure video consultation, the provider will conduct a comprehensive assessment based on standardized criteria. This may include discussing your symptoms, medical history, and any relevant behaviors.
4. Receive Diagnosis and Personalized Plan
If diagnosed with ADHD, you'll receive a signed diagnosis letter and a personalized treatment plan. Treatment options may include therapy, success coaching, and non-stimulant medication management.
5. Ongoing Support
ADHDAdvisor.org offers continuous care through various services:
- Medication Management
- Therapy Sessions
- Success Coaching
All services are HIPAA-compliant, ensuring your privacy and confidentiality.





.svg)